Connect With Us
Blog
Blog
The Odd Sensation of a Morton’s Neuroma

Morton’s neuroma, or interdigital neuroma, is a painful condition caused by the thickening of tissue surrounding one of the nerves in the midfoot, often between the third and fourth toes. This irritation results from nerve compression, frequently due to repetitive stress or pressure from wearing tight or high-heeled shoes. The condition can feel like a sharp, burning pain in the ball of the foot, often radiating to the toes. Some patients describe it as feeling as though they are standing on a pebble, or having a clicking sensation. Risk factors include high-impact activities like running, foot deformities such as bunions or flat feet, and poor footwear choices. Diagnosis often involves a physical exam, an ultrasound, or an MRI scan. Treatment ranges from modifying footwear and orthotics to corticosteroid injections or, in severe cases, surgical removal of the affected nerve tissue. If you have this odd and painful sensation in your foot, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Painful Ingrown Toenails

An ingrown toenail occurs when the edge of the toenail grows into the surrounding skin, leading to pain, redness, and swelling. This condition commonly affects the big toe and can be caused by improper nail trimming, wearing tight shoes, or injury to the toe. Symptoms typically include localized pain, tenderness, and, in some cases, drainage of pus, indicating an infection. If left untreated, ingrown toenails can lead to more serious complications. Initial relief options include soaking the affected foot in warm water, gently lifting the nail edge, and wearing properly fitting shoes to relieve pressure. However, if the ingrown toenail persists, becomes infected, or causes severe pain, it is important to see a podiatrist. This type of doctor may recommend antibiotics or a minor surgical procedure to remove the ingrown portion of the nail. If you are experiencing discomfort from an ingrown toenail, it is suggested you schedule an appointment with a podiatrist for an accurate diagnosis and effective treatment options.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Are Bunions Affecting Your Everyday Life?
The Impact of Diabetic Foot Ulcers on Quality of Life

Diabetic patients with foot ulcers can experience significantly reduced quality of life due to chronic pain, limited mobility, and the risk of serious complications like infection or amputation. These ulcers, often caused by poor circulation and nerve damage, can make everyday activities difficult and may lead to prolonged hospital stays or social isolation. The emotional toll, including stress and anxiety, further impacts their overall well-being. Managing foot ulcers in diabetic patients requires a comprehensive approach. Regular foot exams by a podiatrist, proper wound care, and the use of custom orthotics or footwear can help reduce pressure and promote healing. Blood sugar control is critical in preventing further damage. In more severe cases, advanced treatments like hyperbaric oxygen therapy or surgery may be needed. If you suffer from diabetic foot ulcers, it is strongly suggested that you include a podiatrist on your team of healthcare providers to improve functioning. Education on daily foot care, combined with early intervention, can help prevent ulcers and improve your well-being.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Misdiagnosed Foot Pain From Cuboid Syndrome

Cuboid syndrome occurs when the cuboid bone becomes partially dislocated. It is often misdiagnosed because symptoms like pain and discomfort along the outer edge of the foot resemble other foot conditions. This condition commonly affects ballet dancers and athletes due to the repetitive strain they place on their feet. Predisposing factors include poor foot biomechanics, ankle sprains, or improper footwear. Symptoms include sharp pain along the outer side of the foot, difficulty walking, and tenderness when pressure is applied to the cuboid area. Treatment often includes manual manipulation to reposition the cuboid, rest, and the use of orthotics to support foot alignment. If you have lateral foot pain, it is suggested that you visit a podiatrist for a proper diagnosis and appropriate treatment.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
- Injury – The most common cause of this ailment is an ankle sprain.
- Repetitive Strain – Tension placed through the peroneus longus muscle from repetitive activities such as jumping and running may cause excessive traction on the bone causing it to sublux.
- Altered Foot Biomechanics – Most people suffering from cuboid subluxation have flat feet.
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Alignment Problems in Children

Pediatric foot alignment deformities are common conditions in growing children and can affect how their feet develop and function. These deformities include flat feet, where the arches do not form properly, or conditions like in-toeing, where the feet turn inward. These issues often arise from the natural development process or genetic factors, and in most cases, children outgrow them without treatment. However, when foot alignment deformities cause pain, difficulty walking, or limit a child’s activities, they may require medical attention from a podiatrist. Treatment options can include stretching exercises and custom orthotics to correct the alignment and relieve discomfort. If you have a child that is complaining or showing foot discomfort, it is suggested that you schedule an appointment with a podiatrist to help monitor the condition and determine if any treatment is necessary to support healthy foot development in the growing years.
Making sure that your children maintain good foot health is very important as they grow. If you have any questions, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Keeping Children's Feet Healthy
Having healthy feet during childhood can help prevent medical problems later in life, namely in the back and legs. As children grow, their feet require different types of care. Here are some things to consider...
Although babies do not walk yet, it is still very important to take care of their feet.
Avoid putting tight shoes or socks on his or her feet.
Allow the baby to stretch and kick his or her feet to feel comfortable.
As a toddler, kids are now on the move and begin to develop differently. At this age, toddlers are getting a feel for walking, so don’t be alarmed if your toddler is unsteady or ‘walks funny’.
As your child gets older, it is important to teach them how to take care of their feet.
Show them proper hygiene to prevent infections such as fungus.
Be watchful for any pain or injury.
Have all injuries checked by a doctor as soon as possible.
Comfortable, protective shoes should always be worn, especially at play.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Avoiding Foot Pain

Foot pain can present as aching, sharp, or burning sensations in the heel, arch, toes, or ball of the foot. It can be caused by various factors, including wearing poor footwear, overuse, flat feet, high arches, or conditions like plantar fasciitis, bunions, and arthritis. Injuries like sprains or fractures also contribute to foot pain. Foot pain can impact other parts of the body by altering gait and posture, leading to knee, hip, or lower back discomfort. This occurs when the body compensates for pain by shifting weight improperly. To avoid foot pain, the first step is wearing well-fitted, supportive shoes. If your foot pain persists, worsens, or affects your mobility, it is suggested that you schedule an appointment with a podiatrist as early intervention can prevent complications and improve overall foot health.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Heel Pain Can Be Treated!
Symptoms and Causes of a Broken Pinky Toe

A broken pinky toe, or fifth metatarsal fracture, often results from trauma or injury. Common symptoms include immediate pain, swelling, bruising, and difficulty walking. The pain can be sharp and may worsen when pressure is applied, such as wearing a shoe. A noticeable deformity or inability to move the toe can also indicate a fracture. The primary causes of a broken pinky toe are accidents such as stubbing the toe, dropping heavy objects on it, or direct impact during sports. Poorly fitting shoes or high-impact activities can increase the risk of injury. Prompt treatment is vital for proper healing. If you have fractured your pinky toe, it is suggested that you contact a podiatrist.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Caring for Corns on Children’s Feet

Corns are small, thickened areas of skin that develop on children's feet due to pressure or friction, often caused by wearing poorly fitting shoes. They typically appear on the tops or sides of toes or on the soles. While not usually dangerous, corns can cause discomfort or pain, especially when walking. To manage corns, parents should ensure their child's shoes fit properly, offering enough room for toes to move freely. If a child has diabetes or circulation issues, complications from corns can develop as their feet may be more vulnerable to infections or other foot problems. It is suggested that you consult a podiatrist if the corn persists or worsens.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
More...
A Guide to Types of Running Shoes

Selecting the appropriate running shoe is vital for both comfort and performance. There are several types to consider. Neutral running shoes offer balanced support and cushioning for those with a neutral gait. Stability shoes provide additional support for runners who overpronate or roll their feet inward excessively. Motion control shoes are designed for severe overpronation, offering maximum support and control. Trail running shoes feature rugged soles and enhanced traction for off-road conditions. When choosing the right shoe, consider factors like your foot type, running style, and the terrain you will be covering. It is also beneficial to try on different styles, as properly fitting shoes can prevent injuries and enhance your running experience. If you have endured a foot or ankle injury while running, it is suggested that you consult a podiatrist who can offer treatment options, in addition to guiding you on the right type of shoes to wear.
You should always make sure your running shoes fit properly in order to avoid injury. For more information, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Choosing the Right Running Shoe for Your Foot Type
Improper shoe sizing can cause a myriad of problems for your feet. Shoes that don’t fit you properly can lead to muscular imbalances in your body, which can result in foot, knee, and hip injuries.
Tips for Finding the Right Running Shoe
- Make sure you have a thumb’s width of wiggle room between the end of your longest toe and the front of the shoe.
- There should be little to no slipping at the heel
- Don’t assume your size in one shoe brand will be your size in another
- Do not lace up your shoes too tightly
- Walk around in the store with your new shoes before you buy them
If you have any questions please feel free to contact our our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The Importance of Diabetic Foot Exams

A foot exam is important for preventing complications and maintaining foot health in individuals with diabetes. During the exam, a podiatrist will assess various factors to ensure early detection of potential issues. Key areas of focus include checking for any cuts, sores, or infections, as well as examining the condition of the skin for dryness, cracks, or fungal infections. They will also evaluate circulation by checking pulse levels in the feet and legs, and test sensation using a monofilament or tuning fork to detect any loss of feeling. Symptoms like persistent pain, swelling, or changes in skin color can indicate underlying problems that require attention. The exam may also include a review of footwear to ensure it provides adequate support and minimizes pressure points. To keep your feet healthy and address any concerns promptly, it’s suggested you make an appointment with a podiatrist for a comprehensive diabetic foot exam.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Risks of Plantar Fasciitis in Diabetic Patients
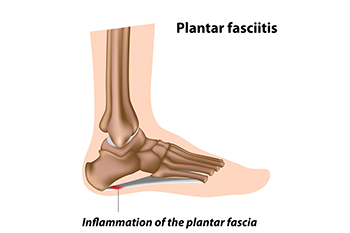
Plantar fasciitis is common among people with diabetes, worsening foot problems due to compromised blood circulation and nerve damage. This condition involves inflammation of the plantar fascia, a thick band of tissue stretching from the heel to the toes. In diabetic patients, factors such as poor circulation, neuropathy, and improper footwear can increase the risk of developing plantar fasciitis. The condition primarily affects the heel and the arch of the foot, causing sharp, persistent pain, especially noticeable with the first steps in the morning or after periods of inactivity. Managing blood sugar levels and choosing appropriate, supportive footwear are essential in reducing the risk and alleviating symptoms of plantar fasciitis in those with diabetes. If you have diabetes and are experiencing heel pain, it is suggested that you are under the care of a podiatrist who can treat plantar fasciitis and help you manage complications of diabetes.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Warts Can Be Treated!
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019



